Forum Replies Created
-
AuthorPosts
-
-
2023-07-24 at 4:28 pm #41317
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipant1. What factors contribute to the high incidence of drug-resistant Tuberculosis in an area?
To answer this question generally, in Thailand, I’ve found that drug-resistant TB most commonly results from inappropriate use of antibiotics. I also recently found out that “Levofloxacin”, which also one of the alternate regimen for MDR-TB, is also openly sold in some pharmacy store without prescription for “sore throat”. It is highly possible that in the future, there will be much more incidence of antimicrobial resistance.2. If your living area is identified with a high risk for MDR-TB, what is your idea (regarding intervention strategies) to reduce the risk?
I think we should identify and isolate those who have MDR-TB and put the resistant-strain on watchlist. -
2023-07-11 at 4:54 pm #41257
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantSorry for late response.
This is my dashboard displaying COVID-19 statistics in 6 countries. The charts illustrate accumulative patient count between year 2020 to 2022. Filters include country and date range. Data mainly showed cumulated cases, deaths and recovered cases. Two charts are included in the dashboard. The chart located above shows trends for each case by date. The bar chart below is drivable between number of cases by year and selected countries. -
2023-07-01 at 10:37 pm #41185
-
2023-05-21 at 3:50 pm #40616
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantYou did a good work. I do, however, have a few things to suggest about your CRF.
The screening part is mainly about inclusion/exclusion criteria, right? There are spaces between each item and it may confuse someone whether there should be any information filled inside them (date of vaccination or other thing).
There should also be a separate section clearly state that this subject is eligible for trial or not in case the reviewer is trying to figure out who to include in the trial.
The local reactions should have an optional field in case there is any other reaction occurred.
The laboratory section, the WBC item should be in _____ x 10^n cells/mm3 instead of ____ / mm3. An influenza antibody (hemagglutination) titre consists of subset of strains, you may want to include them as well.This is only my personal suggestion. Please feel free to correct me if there is any misunderstanding.
Thank you.
-
2023-05-13 at 10:44 pm #40546
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantDate of informed consent and date of birth would be great if they are properly labelled as
______ / ______ / ______
(Date) (Month) (Year)Without label, how would you know whether which format they intent to fill.
Take this for exampleDate of birth: 05/04/1989
Is it 5th April 1989 or 4th May 1989 ??
Not all people write date in DD/MM/YYYY format, right? Some may prefer MM/DD/YYYY. we don’t know.
So it’s best to predefine the format and explicitly write down to guide whoever fills this form. -
2023-05-13 at 10:39 pm #40545
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantCan you give me 1 example about the benefit of having data standards for clinical research?
Data standards in my point-of-view can be seen as if they are syntactically defined languages, making data transfer and utilisation more robust and efficient. Especially in almost every step in data management process. For example, let’s say you want to fetch some data from different hospitals with different HIS system. You want laboratory tests about CBC. Hospital A gave you a dataset exported directly from their database. In reality, you won’t get a plain text that write both values and units of measurement
e.g.
Row 1: Total WBC 12,500 cells/mm3
Row 2: Total WBC 8,900 cells/mm3
Row 3: Total WBC 15,200 cells/mm3but instead you got this:
Row 1: 12500
Row 2: 8900
Row 3: 15200So.. with these numbers, you wouldn’t know which unit of measurement they are originally stored in because some hospitals might store in a different unit.
The real problem occurs when you get to work with many datasets and you couldn’t possibly simply make a guess. That’s why having data standards with consensus in organisations will help solve this problem.
-
2023-05-13 at 10:23 pm #40544
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantTo ensure data quality and integrity, the data management process should have the following process.
– Audit trial/Time stamp
– User authentication and access control level
– Edit check and logical check
– Data backup and recovery plan
Do you have experience conducting a study (or have seen other study projects)? Do those projects have implemented these process? Which computer software that you/they use to store and manage data?I’d like to share my previous experience about research data management. In my opinion and experience, I think data backup and recovery plan are the most important. The reason why is that when something was wrong and you lose all the data, everything you’ve done so far was for nothing. I used 3-2-1 backup strategy for very important data. Here’s the brief description of what 3-2-1 backup strategy is.
The 3-2-1 backup strategy simply states that you should have 3 copies of your data (your production data and 2 backup copies) on two different media (disk and tape) with one copy off-site for disaster recovery
I find this technique as a very effective way of backing up data as well as safeguarding them. I have one copy of working data on my machine [Copy #1] (I use macOS and have its back up tool set up; it’s called Time Machine where your data is automatically backed up periodically to an external hard drive [Copy #2]). After I finished working with these data, I also uploaded them to Google Drive [Copy #3] for further use and collaboration with other team members. When my project has finished, I archived them in 1) my personal machine (and of course, Time Machine) 2) Compressed archive on google drive 3) my personal NAS (Network-Attached Storage)
This way I can make a copy of my research and lifelong work safely.
-
2023-05-05 at 8:53 pm #40218
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantBased on your experience in data collection/management, which steps in the data management workflow that you have done and have not done?
If you have a chance to go back, which steps that you should have done it to improve your project?Our research back then, it was our first research which we designed from the beginning.
In the study initiation phase, what we have done were
(1) protocol discussion with our group and our advisor, using previous research paper as guideline.
(2) data collection design (based on existing, validated questionnaire)
(3) data acquisition (paper-based CRF)However, without prior knowledge on how to systematically conduct and comply with the data management process, we did not explicitly declared on data management plan. We only collected paper-based CRF, enter them into online collaborative spreadsheets and into SPSS software. We also did not plan thoroughly about where to keep them. It was a mess back then when we don’t know which was the latest version of data, etc.
Luckily, because the scope of our research was not large, it was handled without any problems.(4) Database access control -> Like I have mentioned earlier, our data was digitised from paper-based into shared spreadsheets. We used a built-in tool which help us define who has the designated role to view, access or edit our data. Edit Check Type was handled manually.
Moving on to the next process, we had done both data entry/processing and data validation steps 🙂
In the project closure workflow, regarding our study protocol, SAE Reconciliation and external data merging were not mandate. After we finished entering data into digital spreadsheets, we downloaded them and use those data locally with our statistic software. The original CRFs collected were photographed, archived locally and disposed accordingly.
-
2023-05-05 at 8:24 pm #40217
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantI’d like to share my past experience about data collection while I was in medical school. I was part of a research group and we conducted research with our assigned advisor, a gynaecologist. The research was about the prevalence of GERD (Gastroesophageal reflux disease) in pregnant woman in Maharaj Nakorn Chiang Mai Hospital.
1. Purpose of data collection
For research purpose.2. Was it primary or secondary data collection?
Primary data collection directly from data sources (patients visited at OB-GYN department)3. Methods used for data collection
A paper-based case record form (questionnaire) was used. There was previous study which utilised GERD-Q score to evaluate symptoms of GERD quantitatively. It was originally in English. We translated them and had the translated version of questionnaire verified and validated by three experts in OB-GYN field.4. Were there any problems that occurred regarding data collection?
There sure are. Mostly about the data quality obtained. First, and I believe this is the most common problem found in almost every research, was a missing data. Incomplete questionnaires were returned, and there were plenty of them. Some subjects may omitted some part of the question, or skipped them. Second, some of our subjects needed clarification and we need to spend extra time to explain every single one of the questions provided despite our limited manpower. (we had only four members, and around 20 patients took the test simultaneously). Cooperation was one of the problems we encountered. Fortunately, there were not so many patients who denied to take the questionnaire. -
2023-04-24 at 10:32 pm #40063
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipant
-
2023-04-24 at 10:22 pm #40062
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipant
-
2023-04-09 at 6:45 pm #40014
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipant
-
2023-03-26 at 10:15 pm #39937
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantPoint 23rdPage 8 (344)
If one 95 % confidence interval includes the null value and another excludes that value, the interval excluding the null is the more precise one.
Believe it or not, I do always believe this exact concept until now.
By the above misconception, people sometimes misunderstood that if a confidence interval (CI) includes a null value, the other CIs which exclude null values are more precise. But in reality, what defines precision is actually the CI “WIDTH”. The lower and narrower CI width means that it is more scoped and more precise even the lower CI width includes a null value. -
2023-03-11 at 10:55 pm #39750
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantIn the world of data-driven era, big data and advancement in technology makes analysing a large quantity of data happens at a glance.
The extent to which data is identifiable depends on the number of subjects with those identifiers. In health data, we have HIPAA act which mainly focused on privacy issues. Let’s have a look at this for an obvious example!
Imagine that we are talking about elderly with an age of 90. How many of people nowadays who live that long, a thousand around the world? Maybe. But if we specify the location, such as male, age 90, who lived in Amphor Mae Sa Riang Chiang Mai, you may have just one or two person.
Another example, a guy from Chiang Mai, graduated from Faculty of Medicine. Age 26. Currently study MSc at Mahidol University. Without the name of a faculty — if you asked one of my friends, they will instantly know that that was me 😂
FYI, for those who interested in HIPAA, you can look up about it more here
https://www.hipaajournal.com/considered-phi-hipaa/What are the 18 HIPAA Identifiers?
The 18 HIPAA identifiers are the identifiers that must be removed from a record set before any remaining health information is considered to be de-identified (see §164.514). However, due to the age of this list, Covered Entities should ensure that no further identifiers remain in a record set before disclosing any health information to a third party (i.e., for research). The 18 HIPAA identifiers are:Names
Dates, except year
Telephone numbers
Geographic data
FAX numbers
Social Security numbers
Email addresses
Medical record numbers
Account numbers
Health plan beneficiary numbers
Certificate/license numbers
Vehicle identifiers and serial numbers including license plates
Web URLs
Device identifiers and serial numbers
Internet protocol addresses
Full face photos and comparable images
Biometric identifiers (i.e., retinal scan, fingerprints)
Any unique identifying number or code -
2023-03-11 at 10:38 pm #39749
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantThe very first thing that came up into my mind and I believe, most of the time, when you are facing some problems which is hard to figure out is to ask! That is probably be the same as this case. However, this task can not simply done by just asking questions in a larger population. We need a systematic way to explore such problems..through research!
In this case, I may start with some review about this bednets system whether about how it is built, what it does, platform availability, target users’ information, etc. After we have identified essential topics about them, then we could start by deploying a simple questionnaire consists of multiple questions which could be the validated questionnaire –– TAM, for instance. This is called a cross-sectional (conducted in one point of time), quantitative (measurable) research. After that, we can skim through responses and we may conduct further focus group discussion in order to explore insights in the particular group with extreme response, for example, lowest possible score in some aspect or areas by using an open-ended question. Nonetheless, we need to predefine and anticipate possible confounder factors, biases to ensure an integrity and quality of the research.
-
2023-03-11 at 10:21 pm #39748
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantIn order to adopt a new technology in place of the old one, you have to make sure that the new technology you are adopting will definitely help users accomplish their tasks more easier. That’s where TAM comes in to help us with. It is basically a quantitative way to measure users’ acceptance using multiple questions in a scale of 1-5 or 7 depends on its version, apparently. After piloting the new technology, it is essential to obtain users’ voices or opinion periodically, and eventually evaluate the new technology prior to discarding the old one. The original TAM measures two core factors including Perceived usefulness and Perceived ease of use, which I have mentioned earlier in the previous discussion 🙂
-
2023-03-11 at 10:12 pm #39747
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantWhat are some specific ‘external variables’ that you think might influence an individuals’ perceived ease of use or perceived usefulness of a new technology?
I am currently working on research about the technology acceptance model (TAM). The original proposal behind the idea of this model was that an individual’s behavioural intention to use a particular system consisted of two beliefs (i.e., two constructs) which were Perceived Usefulness (PU) and Perceived Ease of Use (PEOU). However, more recent studies showed that those two key elements are also influenced by other factors, including external factors which are (1) social influence, which refers to how people around the individual think and decide. Such opinion has an impact to one’s perception about the new technology and hence, and acceptance. The latter is (2) organisational support, if the individual has received sufficient training and support alongside the new technology deployment. It would significantly attenuate resistance to change.
Other factors include the perception about privacy, security and also technology/digital literacy. It is obvious that younger generations have more opportunity to access digital technologies than previous generations. They grew up with them and frankly are more familiar with them. -
2023-03-11 at 9:57 pm #39746
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantThe terms efficacy and effectiveness are frequency used in health care. The first term, efficacy is the ability of a treatment to work in ideal or controlled conditions, whereas effectiveness is the ability of a treatment to work in real-world settings.
Efficiency, on the other hand, is a term referred to the ratio of the output to the inputs of any system. It is commonly used term in an economical aspect (i.e. cost-effectiveness of the intervention and an outcome) . To give an example, a high efficacy drug in trial might be high, yet the cost spent on the treatment is no superior than the conventional treatment. Thus, it is not considered efficient, or not cost-effectiveness.
-
2023-03-09 at 5:21 pm #39743
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantIn a study to determine contact patterns in Thailand, people were encouraged to use a contract tracing application over a 3-month period. The researcher found that young adults had the most active contact pattern than other age groups. Please help identify confounders for this association. Please provide one confounder for each student, and please try not to duplicate your friend previous answer.The first thing that came up in my mind was users’ age. To declare, young adults could possibly have more ease of access and more comfortable using mobile application. It might be the reason why they contributed to most of the users, hence, the people entering information into the application. Other thing could be their lifestyles. Young adults are of the age of working, outgoing, interacting with more people.
Previous comments from our friends give a great example of the confounding factors! Very interesting.
-
2023-02-06 at 9:28 pm #39642
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantChoose one (or more) of the following vital statistics and describe
1. Definition of each vital statistic?
2. How to calculate each vital statistic?
3. What are the main usefulness of each vital statistic?Here is a list of vital statistics.
Case-Fatality rate
Mortality rate
Age-specific mortality rate
Maternal mortality rate
Infant mortality rate
Neonatal mortality rateLet’s start with the first one,
Case-Fatality rate (CFR)
Its definition is the proportion of people diagnosed with a certain disease and died from that specific disease without time period between disease onset and death taken into consideration. This indicator often reports as percentage and measures the disease lethality.
The calculation of the CFR = [(No. of deaths from the disease) / (No. of confirmed case of the disease)] x 100Other indicators provided in the example mostly focused on the mortality rate.
The mortality rate is different from the CFR and sometimes may cause confusion. The mortality rate is a measure of relative number of deaths (whether by a specific disease or in general) within the PARTICULAR POPULATION per unit of time from ANY CAUSE
It is typically expressed in units of deaths per 1000 individuals
The numerator for the mortality rate is [(No. of death) / (Population of that area)]Unlike other measurements, such as perinatal/maternal/infant mortality rate which are more specific to the particular causes, hence their names. The numerator and denominator are also different, yet stand with the fundamental idea of the
mortality rate. -
2023-02-06 at 1:28 am #39634
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantI see many fabulous work and interesting point of view from you guys! So impressive and comprehensive. Thanks!
For me, as a physician, my current and perhaps forever job would be treating patients! Like many of our doctor friends here said, “First, Do No Harm”. I have treated most patients the same way without taking the patient’s socioeconomic status as a judgement of providing treatment. However, in reality, they may have some limitations that we cannot provide the ultimate treatment for all of them whether the limited budget or resources, yet the minimum life-saving condition must be given at all costs.
Clinical Practice Guideline (CPG) is the ultimate guide for the practitioners. It is approved for use and adjusted for use in the specific context, depending on the availability of budget and resources. Some CPGs might not be suitable for other contexts, but it is the best choice we have to properly allocate the limited resources. I often follow them, because
1. It provides an optimal outcome for the patients
2. It can be use for reimbursement
Some patients may need special or extra treatment, then I sometimes readjust the treatment differently from the provided guideline. In order to do that, the hospital needs to pay for the extra cost themselves. Giving the hospital administrator a proper and enough reason, it can be exclusively permitted on per-case basis. -
2023-02-06 at 1:04 am #39633
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantPlease share about the work towards the UHC scheme in your country, what works and what needs to be done to make it work, strength and weakness, for example. (10 marks)
The UHC scheme in Thailand (or a.k.a 30-Baht Scheme / Gold Card / UC – Universal Coverage) is a well-known scheme that brings healthcare access, the fundamental rights, to all Thai citizens as long as you have a valid citizen ID. The current scheme allows people to have a health care access 24/7. For the basic OPD visit or IPD visit, patients have to register for the main hospital of their choice. This usually is the regional government primary health care institution located within their living location zone. One of the misconception is that they can NOT just walk in to essentially ANY hospital they preferred unless they have been referred by the physician if the condition is too complex or too critical to handle. An exception is the emergency condition (aka. UCEP) where the patient can go to the nearest hospital if they are in the specified eligibility list of emergency conditions.
It is already work, it worked well so far and I think it will continue to work. I can’t imagine the situation where sick people do not have access to an even basic human rights. However, this scheme has brought a substantial workload to the health care providers in order to provide a quality of care for every one. The main reason is that people in Thailand, to be honest, somewhat possess a mindset that the health care system is “too easy” to access. Imagine that the hospital needs to handle thousands, if not hundred, patients a day (depends on the size of the hospital, apparently) so to visit just a simple condition like a common cold, you’ll have to wait hours before seeing the doctor, and extra hours for waiting for the medications. This simple process might take a whole day for some hospitals. Then there are some patients who do not wish to wait for this process, and instead, they come with the regular, not emergency, condition in the Emergency Department in the middle of the night for some painkillers, for instance. That’s the problem we now face every day.
To be specific for what needs to be done… well, like I said, there are so many benefits provided to every one for the basic rights, this is the main strength! However, it needs to be readjusted and more strict to what kind of condition before they can have the health care encounter to reduce the workload of unnecessary patient visits. Also, the budget distribution and reimbursement from the government needs to be managed wisely in order to continue this scheme further.
-
2023-01-30 at 1:40 pm #39595
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantIn your opinion, what is the situation of health informatics workforce in your country? What are the challenges regarding this issue?In Thailand, we probably have heard terms about “data, big data” more frequently in past few years. The trend about data-driven decision becomes more and more popular. In health care sector, most data collected from the HIS system is still managed and maintained mostly by system administrator — specifically the IT personnel. Hence, the data is neither being used nor utilised. One of the reasons is that it is a data about health care and other professions won’t understand them, not to mention the privacy and confidentiality concerns.
This situation has been like this for decades, until the Health Informatician emerged and filled the gap between them.
It is a work in progress and requires training by multidisciplinary team to create a health informatician. It also is a new field of study where not so many institutions offer a proper training programme. Saying that we are the pioneer in this field is rather not overrated. I agree, as well as many of you that one day we will become well-known and being recognised by people in the very near future. -
2023-01-30 at 3:19 am #39592
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipant“If you are in charge of a data set from your country, will you be thinking about data sharing and why?” (10 marks)
This is a very interesting question. As of today, we are living in the world driven by data and they are undoubtedly invaluable whether in any form or format. In other professions, data can help them make a decision, research purposes, prediction and so on. There are data which can be shared publicly and some can not be disclosed. Health care data is one of the sensitive data and can not be freely shared without rules or regulations. There is a regulation which regulates us on how to share health care data for educational purposes and research with respect to data privacy and security.
The Health Insurance Portability and Accountability Act (HIPAA) is a federal law that required the creation of national standards to protect sensitive patient health information from being disclosed without the patient’s consent or knowledge.
So, to answer the first question, I will definitely thinking about sharing health care data set WITH REGARD TO THE REGULATION. Like I have mentioned earlier, data plays a crucial role in knowledge advancement and if there is a lack of data, you won’t have a research study or any decision making tools.
Unlike other data sets, health care data sets are very tricky because we need to deidentify and anonymise the patients’ detail so that the specific person for that data can not be reidentified by the published data set. This way, we can publicly share the data set for educational, research use. -
2023-01-23 at 4:34 pm #39545
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantUsing EMR instead of the traditional paper-based medical records has various advantages. Especially we are currently living in the era of “data-driven decision”, digitising the data gives us an opportunity to utilise them without having to use manpower alone.
Let’s start with the advantages of using EMR instead of paper-based medical record first.
– Improved efficacy and patient care deliveries — unlike traditional paper-based medical record where doctors and staffs are needed to fill in the physical form, the data is instantly available after form submission by any staffs who need to use them.
– Decrease legibility problem — as many of you may have heard that some physicians’ handwriting are very hard to read, typing them in a computer will certainly help with this problem!
– Improved data archive efficiently — data is stored in a digital format, so there is no need to keep them in an enormous pile of paper, which can pose a significant risk of catching fire. Also, it can be backed up periodically and send to other places rapidly.
– Increased data utilisation — data collected via an EMR, if collected properly, it can be easily used without having to manually review the paper and fill them in the computer over and over again.
– Improved data security — if data governance is properly applied, we can ensure that the data is stored securely with only authorised level of user can access.What about the disadvantages?
– The more easier data access, the more dangerous they can be. Especially if the data security isn’t implemented properly or carefully enough, it may lead to data breach and personal data violation.
– People with little experience in digital literacy may struggle at first, or during the transitional period. It may cause distress and lead to reduced patient care efficiency because they need to focus on how to use the new thing.
– The infrastructure of new EMR needs specialised profession to ensure the quality of data, data validation, data integrity, secure data transmission. This includes data engineers, data scientists, computer engineers, network engineers, system administrator, etc. which can be costly.
– Most EMR systems have centralised database and servers, in case they fail, a replica is needed to operate instantaneously to prevent downtime. Also, user support is a crucial part to successful EMR implementation. -
2023-01-23 at 3:55 pm #39544
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantWhat are your suggestions on coping with those challenges? (10 marks)
From the research paper, there were 14 challenges identified in using big data, its application and implementation in the field of health care. There were some important points that this publication addressed, which were;
1. Missing Data – from my experiences in dealing with Thai EMR data (43 Files), missing data is inevitable. The reasons behind them were exactly as this research stated, because of the poor data collection system, omission by clinicians and health care providers including but not limited to nurses, residents and staffs. In this problem, I suggest to redesign data collection method and encourage users to aware of how entering a valid data will be beneficial to them (in research purposes, for instance). After that, there should be data validation process to help verify data quality and data integrity.
2. Selection bias — Because the data collected for big data analysis is primarily based on different hospitals with their own EMR database. To deal with the data biases, pooling data with different hospitals in a different region, or even a national scale would help reduce this problem.
3. Data analysis and training — this issue can be overcome by training a specialised profession in data science with the combination of knowledge in medical field and programming field.
4. Interpretation and translational applicability of results — Data gained from EMR, however, is retrospective data and will ultimately require another research methodology to validate the application for further use in clinical practice. Also, in data science with artificial intelligent models are somewhat known as the “black box” in which the data output can not be proven by the traditional method. For physicians in clinical practice, they often rely on the evidence-based and this new approach of big data analytics using machine learning model might not be easily provide them sufficient obvious evidence.
5. Privacy and Ethical issue — This is a serious concern, and in my opinion, the most problematic issue which causes a significant barrier in big data analytics in health care. Because big data possesses large volume and velocity characteristics, they require the cutting-edge computational resources and hence, we can achieve them with cloud computing. For legal reasons, including Thailand, the government prohibits storing government data (health care data, included) on the cloud due to fear of data being compromised. The only way we can cope with this issue is that we have to ensure that the data being uploaded to the cloud is strictly and follow the HIPAA and security regulations. -
2023-01-15 at 10:03 pm #39490
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantThis discussion topic is indeed very interesting! I’ve always known that there surely are corruption in the health care field of work, but defining and tackling them are the whole next level. Just like other professions, corruptions are undeniably everywhere. Think of them as shades of grey, there are so many level of corruption and it depends on how it is defined, and by whom. In the provided paper from IJHPM, they proposed four steps of addressing problems and initiating a debate on corruption in health system.
First, we need to define the responsible stakeholders and talk about them together. I agree. However, it is very hard and, like the author stated, reluctant to speak about “corruption”, let alone the awkwardness. Who would brazenly admit that they are corrupted, right? It’s not even hard to define key stakeholders and beneficiaries behind the corrupted system. The important point is that as long as there are persons — it could even be your co-workers, for instance, who will benefit from the corrupted system, they will only strengthening the corrupted system even more. The only way to fight is that you will need support from people who are negatively affected by the corrupted system to demonstrate the impact of current situation. In our case, it could be our patients, co-workers, or your superiors. If you have enough proof and support — then you can open the discussion more easily.
Second, prioritise action and analyse why these corruptions persisted. Make a good use of your support and proceed to pursue the issue that has a bigger impact for most people first.
Third, making a holistic view. There will always be the reasons behind every action. Power, money — for whom and by whom. It’s like a strategic chess game. An external investigator may be helpful in this case, and also to help look from a different angle.
Lastly, this paper mentioned about research community for insights about corruptions. Making the data publicly available for transparency and provide third-party organisations to routinely interrogate might even help reduce corruptions.
-
2023-01-15 at 9:03 pm #39489
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantI will discuss about health system in Thailand, particularly in remote areas, or any health care services outside university hospital and/or smaller than provincial hospital.
Here are lists of main concerns and potential improvement
1. Available resources and budget distribution
– Personnel/health care workers — this topic has been an issue over decades, no matter how many new doctors and other health care providers are being graduated every year, there will always be spaces in the system to be filled. Mainly because we aim to provide as much healthcare coverage as possible to everyone. The solution is straightforward — you just have to create more personnel, yet the barriers are also about budget (in training , salary and so on..) and quality control.
– Laboratory technician and equipments — many small hospitals lack an instrument as simple as a CBC (complete blood count). Speaking of the root-cause, it all comes down to “insufficient budget”. The workaround in my opinion is probably by establishing some laboratory nodes in some common area and provide ways for smaller hospitals to collect samples and send them to the nodes. The potential barrier that comes with having many health care institutions would be about an interoperability across the system, which I’m going to talk about in the next bullet.2. Interoperability and unified health care HIS/EHR
– Imagine that you are a health care worker in a remote hospital. What if the patient is referred out to your hospital from the provincial hospital? You can only see the discharge summary and a brief summary of treatment and vice versa. You can not look for the real-time and up-to-date information about the treatment using a different EHR.
– Firstly, every hospital has each own HIS system. All of them are separated and all of the data is stored locally within the hospital itself in a distributed manner. In Thailand, we do not currently have a unified health care system because it is a big change and will certainly affect a lot of stakeholders, especially the company who created a particular HIS system, the cost of creating a whole new system and infrastructure. Also, the employees are used to the old, classic program that has been used for many many years and the point is that they don’t want to change! They always say as long as the old system works, don’t fix it. That’s the challenging barrier — to make people accept the change. -
2022-12-07 at 10:29 pm #39248
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantAccording to CISCO Disaster Recovery Plan Best Practices, they have proposed three core components that should be included in the disaster recovery plan which are,
(1) Identify and classify the threats/risks that may lead to disasters
(2) Define the resources and processes that ensure business continuity during the disaster
(3) Define the reconstitution mechanism to get the business back to normal from the disaster recovery state, after the effects of the disaster are mitigatedIn healthcare settings in Thailand, for example, we have a strong health care system which is able to provide almost sufficient care to the majority of people comparing to many countries. Unfortunately, a disaster is one of the risks which may lead to a devastating data loss yet potentially preventable. There are various types of disasters depending on the area whether it might be flooding, fire (caused by lightning strikes, short electrical circuits, heat, etc.), accidental damage, earthquake, and so on. After certain risks have been estimated and evaluated, we have to determine the risk by using a risk assessment matrix. Then we must identify stakeholders and related committees in case the situation occurs.
Most hospitals in Thailand, they tend to keep all the data locally in the centralised database located in their very own hospitals. If anything happens, be a flood or fire, even they have a back up or replica in place, it would not be of much help. The problem is that there are rules clearly stated that a government data must not be kept on the third-party cloud. In this case, I suggest that each hospital should have another backup elsewhere which is not located in the same region or risky location. It could be a data centre of the MOPH or anywhere. However, the cost of maintaining a centralised database for such amount of healthcare data is very high, but the safety of the invaluable data is worth the price.
-
2022-12-01 at 1:47 am #39234
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantSorry for late response!
High availability technology is a very useful technology these days because it can effectively manage, distribute and ensure the availability of important data. For RAID technology can make a redundancy by utilising array of drives (depending on RAID type). If you need your data to be highly available and that data is too important and you cannot effort any risks of losing them, for example, patient history and medical records, billings — almost everything! Then, RAID (RAID-1 or higher) may be considered for use. In that case, it will certainly benefit both patients and hospital because there will be no interruptions delivering patient care. However, it might come with an additional cost for setting up a high availability system, but in the long run; it will ultimately provide a strong data protection in the future. Load balancing also ensure that the workload of data access is evenly distributed to all servers to reduce performance impact on a single node and thus, reducing delay in accessing data from users.
-
2022-11-22 at 10:09 pm #39175
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantI have the exact same problem with what Mr.Kawin said! It’s about the default password and “test” password which I believe was once created to simplify internal testing yet those accounts still are active in real world use. Nonetheless, I have never really had any direct experience about CIA in my organisation. Well, there might be some “downtime” in the HIS server due to power shortage, malware attacks but other things seem to be performing well to me. All hospital data is stored within internal network and is not intended to be shared whatsoever, but since it is an old-fashioned database design which was used over decades ago, I strongly doubt that it will provide such an encryption or data privacy policy, to be honest.
In order to achieve data confidentiality, integrity and availability standard, I personally would suggest to upgrade an infrastructure and database design, but I don’t think it is something that can be done over night because it will require a lot of manpower, time and resources.
-
2022-11-22 at 5:20 pm #39173
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantReflect and report some factors related to healthcare resources during the pandemic, categorized by a STEEP letter in your setting.
Imagining I’ve been working for the government healthcare sector, monitoring all healthcare resources in Thailand, A scenario planning strategic — STEEP (which stands for Social, Technologies, Environment, Economic and Political, respectively. ) is a tool to help us determine any potential factors which affect our results.
Social
– Social distancing policy has been enforced, so any physical contact is greatly reduced.
– People tend to believe fake news from communication platforms, including text messaging and gossips. Especially about an alternative remedy, pseudoscience without a solid evidence, or Anti-vaxxer.
– Some people may hoard, store and stock supplies, especially food, medical masks or medicines for their own purposes.Technologies
– Technologies have become even more advanced during an epidemic, especially in telecommunication because of the lockdown and social distancing.
– Government sectors, healthcare facilities and researchers mainly focused on developing a solution for an epidemic.Environment
– Use of healthcare devices and equipments increases, producing more waste to the environment. For example, a disposable glove, plastics, disinfectants. All of which may produce traces behind and not completely recyclable.Economic
– There was once an imbalance of supply and demand in Thailand during an epidemic. People who have economical advantages can possess more resources.
– During an epidemic, global economic slows down to channel funding to research and healthcare problems (most countries, I believe). People don’t simply want to spend their money and save them for urgent matters.Political
– Various policies by numerous parties were advertised in order to gain popularity and support even some of them were not pragmatic regarding the available resources.
– Some government might not even consider the epidemic an important matter, instead, they may focus and invest on things such as economy, military, gaining power rather than supporting healthcare and research until it was too late and the outbreak was out of control. -
2022-11-13 at 9:51 pm #39102
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantYour presentation explicitly addresses the importance of snakebite victims its consequences very well.
I also have seen a LINE group which has been created by a volunteer group of people (Hotline LINE Snake in the house; สายด่วนงูเข้าบ้าน)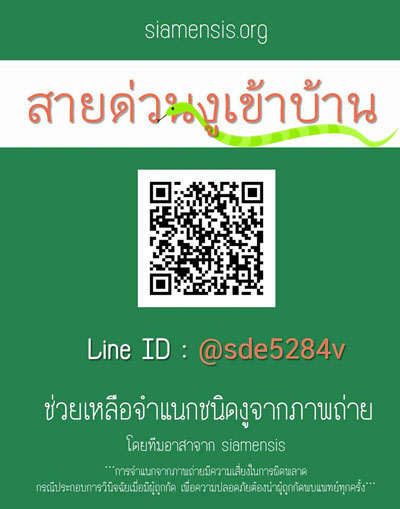
They can identify type of snakes by sending them a picture and they will usually respond within 5-10 minutes. It is also a good opportunity to work with this group owner if possible (just the idea), so that if there is any venomous snake reported – they might be able to provide you a location from where the snake is being spotted and then alert a surveillance system to warn people in the nearby area to become aware.
Your presentation also provides detail on how to collect data as a measurement for quality domains! Very useful.
-
2022-11-13 at 9:40 pm #39101
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantThank you for sharing!
As I am also doing an assignment in this very same topic, I must say that your presentation is very comprehensive! RSV really is a threat these days, I have seen many children suffered from RSV pneumonia and it was very bad.Your presentation on stakeholders also include community leader and village health volunteer, which are also a great idea to help detecting the outbreak because it really helps reduce the workload for healthcare providers as well!
-
2022-11-09 at 10:54 pm #39074
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantComparing how leaders of the two different countries react to a coronavirus outbreak and how they communicate, there may be some differences but I think they all cover the main point of the principles of CERC after all.
1. Be First
– Singapore PM announced a crisis communication about two weeks after an outbreak had occurred whereas Trump was a little bit late.2. Be Right
– They both provided accurate information with sufficient medical guidance. Singapore PM emphasised on how they actively working on the unknown issue for this matter, including regular briefings, research and so on.
While Trump mostly focused on the government action, restrictions, and too many details with less precision of what message he was actually trying to send.3. Be Credible
– Singapore PM mentioned about which steps that his team were working on and what he was going to do next. Most of the speech were evidence-based. Trump also addressed multiple government sections and actions they have committed but again — too many details and make it hard to grab the main idea and thus make he less credible.4.Express Empathy
– Singapore PM had shown his empathy along with subtle humour (when he was talking about stocking up supplies) and being respectful at the same time. He also stated on fear and anxiety, which were totally normal, yet may do more harm than the virus itself if improperly controlled. His positive facial expression and words that he used also delivered a positive emotion and inspiration. Trump also showed his empathy to his citizens at the beginning.5. Promote Action
– Singapore PM provided necessary steps including hygienes, self-monitoring. He also valued his citizens and reminded that everyone was also an essential part of successful outbreak control. Trump also promoted disease prevention as well. The only difference was that Trump looked far more serious and bold.6. Show respect
– Singapore PM and Trump acknowledged their teams and citizens. One thing that I believe is that Trump has blamed other countries, especially China for the outbreak. -
2022-11-09 at 5:06 pm #39069
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantSorry for a late response…
I’ve been searching through an archive and this is the best I could find
-
2022-11-02 at 10:28 pm #38990
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantEver since the COVID-19 pandemic, Thailand has shown its potential towards a digital health transformation. Many projects and applications have been launched from the government with cooperation from private sectors. All of them have shown promising results. So I think in a theme of
Team, my country is doing incredibly well.Like many classmates from Thailand have stated that our country needs to improve in the theme of “Transparency and Trust” and “Techquity”. Some of the platforms provided by government sector have utilised our personal data for their primary goal, yes, but provided that the political situation and citizen’s perception of the government transparency have become questionable that they might abuse the data.
For “Techquity” theme, even though most people nowadays have been using smartphones, it is an undeniable fact that there are still some places especially in rural areas where technology is still hard to access. The cause is mainly from a different in socioeconomic status, lack of government support and education.
-
2022-11-02 at 9:43 pm #38989
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipant(1) Could you list the disease outbreaks that have been declared as the Public Health Emergency of International Concern (PHEIC) and (2) Why do these outbreaks raise such concerns??
1. 2009 H1N1 pandemic – First index case was observed in Mexico, presented with symptoms resembling influenza. After further investigation, a new strain of influenza virus was identified in the US. It is more likely to raise concern as it has travelled across the states with a high morbidity and mortality.
2. 2014 Polio virus – no wonder why this is one of the most disabling outbreak and results in PHEIC declaration. This virus is highly contagious via faecal-oral route. A large number of people has been affected, causing severe disability across multiple countries before the vaccine become available.
3. 2014 Ebola outbreak in Western Africa and 2018-2019 Ebola, Kivu epidemic – This disease has a high mortality rate and difficult to detect in the first stage of infection. A lockdown has taken place throughout the affected states .
4. 2015-2016 Zika virus – This zoonotic disease is transmitted through the bite of Aedes mosquito family, which could potentially transmit across the country. A series of infant cases born with microcephaly and neurological disease was associated with this disease.
5. 2019 nCoV (COVID-19) – A pandemic with active cases to-date. With its rapid contagiousness and risks of complications in specific population, it has raised a red flag and public lockdown including travel restriction, place lockdown were taken into action.
6. 2022 Monkeypox – transmitted through close contact and cases were identified in many countries, including Thailand.(3) In your opinion, is there a disease or condition that may potentially lead to PHEIC in the future? Why?
I think the possibility of new emerging disease, especially a zoonotic disease can potentially lead to PHEIC declaration. As there is a group of people who are at risk of being exposed to unknown pathogens by going to places like a cave or even seek exotic animals for food. Also, historic diseases may be re-emerge again from climate change or inadequate control and elimination.
-
2022-11-02 at 11:26 am #38974
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantI’d like to share my experience as a leadership role. Back when I was a medical student, I had a chance of becoming a vice president of an international challenge held by my faculty known by the name CMU-IMC. It was such a challenge to me because I have never been in charge of something big like this before. The hardest part was about dealing with different people of different ages. To be honest, it was quite stressful to me because I had to make sure that every thing had to be perfect. I have gained so many experiences from this event and it really matures me.
-
2022-10-26 at 9:33 pm #38864
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantSORMAS system is quite a success from my perspective. It can be deployed with in a short period of time and provided a short training period / low learning curve. I have seen a sample user interface in a provided paper and it is very simple, provides comprehensive visualisation graphics and it has also been used for other diseases as well (as seen in figure 1, there are cholera, dengue, measles, new flu and so on).
Additional indicators for SORMAS in terms of evaluation its effectiveness should be about
(1) User satisfaction; because it has been proven that SORMAS system is superior than the conventional surveillance system. It also has a high potential to be widely implemented in the future for another outbreak to come. By taking user experiences into consideration, the system can improve further.(2) Integration; As the authors stated that they have to deployed SORMAS in the midst of the outbreak without prior plan at the first place, they had to run two separate systems simultaneously. It would be great if we, or anyone, has proposed some kind of “data standard” for outbreak reporting system for interoperability usage regardless of any platform or system they use for outbreak surveillance.
-
2022-10-26 at 8:56 pm #38863
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipant**1. Verification and preparation**
Now that there is the advancement in telecommunication and information technology, most countries have implemented their own health information system and all of which are being regulated and compliant with the central government standard. In most cases, ICD-10 are the preferred standard of sharing diagnosis between health care institutions. Whenever there is any unusual surge in specific symptoms or syndrome, we can easily recognise them beforehand.
**2.Describe the outbreak**
Data visualisation can be implemented alongside with the local hospital database. We can select the specific code for some ICDs and collect insight by reviewing the case if possible. There are many tools which help us deal with numerous data such as Python or R.
**3.Hypothesis and testing**
Simple statistical methods such as risk factors determination, odd ratio, etc. can be easily applied by simple statistic software provided that we have collected enough data.
**4.Response and action**
After we have identified and declared an outbreak, we can quickly set up a response team by a meeting. We have online telecommunication platform such as Zoom, Google Meet, Skype and many others as an alternative to the old-fashioned way. Any decision will be made in a real-time manner and across region, no matter how far they are.
-
2022-10-19 at 9:25 pm #38767
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantThis article gave examples on the application of digital technologies to enhance COVID-19 surveillance and response. Please give 1 technology or tool that you like most and briefly explain how it works and how important it is.
From my personal field, I really am into artificial intelligence. Machine Learning is really popular these days, not that it will replace human but unarguably they are a powerful tools which in turns help us handling a large quantity of data, including COVID-19 data. Processing all of the data, collecting from multiple sources can not be done manually by human alone. Machine learning helps us to analyse those data and more importantly, predictions!
Allow me to introduce one of my favourite innovation and application of machine learning. Screening for COVID-19 from COUGH SOUND (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9138020/). It is something that, say, people from decades ago might say it’s impossible. Now it is. This is just one application from using machine learning, but it may give some of you a bigger picture and see what it is capable of.
-
2022-10-19 at 7:03 pm #38764
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipant1. How can surveillance help to detect and control the disease?
Surveilling is a process of continuously making an observe on a particular matter. A disease surveillance is to observe an occurrence trends, and behaviour of the disease itself, in this case, a monkeypox. It is generally accepted that the faster we know about the disease, the better chance we could timely plan, intervene and contain them.
2. Should we conduct active or passive surveillance or both for the disease, why?
In my opinion, both passive and active surveillance should be conducted as monkeypox is an emerging disease and can spread through intimate contact. The signs and symptoms for this disease can be visible after a few days after contact. A passive surveillance would help detecting a new case in health care institutions and then an active surveillance can be implemented within that area to identify significant contact cases.
3. Which method should be best to identify cases, why?
1. Cases in medical facilities VS community : For monkeypox, eradication of the disease is possible provided that we capture all cases. The symptom is mild yet very contagious, so I think community-based surveillance is suitable to find every single case in a population since the signs and symptoms are very obvious.
2. Sentinel VS population-based surveillance : In my opinion, sentinel surveillance is a way to go here, since the severity of the disease is not high (in other words, low mortality). If people who are at risk or having obvious symptoms, they will likely seek medical attention as outpatients. We can then report back to the disease control sector. It is less costly compared to population-based surveillance.
3. Case-based VS aggregated surveillance : I personally think case-based surveillance is more suitable. As the disease can be transmitted through contact and take at least a few days before the symptoms occur. The total cases are still small and detailed information about their locations and contact are all important in a monkeypox control.
4. Syndromic VS laboratory-confirmed surveillance : In this case, monkeypox symptoms are quite more of a flu-like symptoms. There may be some specific features such as rash over the body. We can screen for potential contact from patients with a non-specific symptoms as it is faster and less costly. So, I will choose a syndromic surveillance.
4. What dissemination tools will you choose to disseminate monkeypox surveillance information? Why do you choose this/these tools?I will likely choose an ongoing, real-time dissemination tools as this disease can be rapidly spread. We are in a data-driven era, and possessing advanced informational technology. This can be done quite easily.
-
2022-10-12 at 11:32 pm #38686
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipant1. Should you give the data out?
Absolutely not! I am not the owner of the data, the patient is. Providing such a detailed information is a major risk that could identify the specific person and sharing that is a violation of a HIPAA regulation.2. How do you not violate any of the general principles of informatics ethics (and) 3. If you want to provide the data to them, what and how will you do it?
First, a research team must fill in an official form and make a request through the responsible organisation. They must disclose their scope of study and state their requirements and data specifications through the ethics committee. Then, the data must be encrypted or de-identified/anonymised/pseudonymised prior to distribution and ensure data safeguarding with the HIPAA rule. -
2022-10-12 at 11:19 pm #38684
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantThis is the most basic patient’s rights! The only answer is NO. Patient confidentiality is what we must respect and it is not our job in the first place. So I would just ignore and continue my work — checking the EMR. I can’t interfere with other people’s issues, even in a “friendly” situation because where I gained this information is because I accidentally found it. I was not even a physician who ordered the test, so I have no right to bring this issue up and talk about it in any way. So, speaking of should my friend not know about this because she might be at risk.. well, to be honest I really think she should have been informed, but like I said, I am in no position to do that as I believe that the physician who ordered this test must have given the husband a choice and prior counselling beforehand. If I were a physician who conducted the HIV test for the husband, I would try my best to convince him to tell his partner (in other word, my friend). That’s the best I can do and I am obliged to withhold that information from any one other than him.
-
2022-10-12 at 11:04 pm #38683
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantI’ll use the project from previous topic, an iSuandok system.
Awareness — During the COVID-19 pandemic, a social distancing measure was encouraged. This system has allowed patients to appoint and receive notifications about their treatment process starting from appointing to medication delivery. Thus, this system has used this issue as an advantage to raise awareness of reduction in social contact as their strength.
Desire — People often want to shorten their time spending in a hospital. Having a system which help them throughout the hospital visit process really saves them a lot of time.
Knowledge — The system is easy to use and user friendly. There are always user manual guide and tooltips provided every where in the application.
Ability — similar to the knowledge section
Reinforcement — this application receives feedback from users and now this system also extends to employees as well. It is integrated to a new EMR system, enabling authorised health care staffs to perform simple tasks such as managing appointments.
-
2023-07-11 at 5:20 pm #41258
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantYour dashboard is very intuitive and user-friendly, allowing viewers to rapidly gathered useful information at a glance.
Great work.
-
2023-06-17 at 10:45 pm #41025
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantI agree with you that the chosen line plots are most suitable for this case. However, those plots are too overcrowded with too much lines (more than the optimum of 4-5 lines) so it’s hard to make people focus on what they want to illustrate. In my opinion, it would be much nicer if they just select plots from the top ten list and discard the rest.
Also, the colour scheme used is too vibrant and lack of carefulness in chosen colour theme. They are not blended and those combinations are just not go well together.
-
2023-01-30 at 1:48 pm #39596
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantI agree with data standardisation. If it is possible to enforce data structure and data standard, that would be ideal. However, HIS for each hospital are designed separately and they often implement their own database structure. Thankfully we have a FHIR HL7 for this purpose. Hope that one day it will be implemented in a large scale!
-
2022-10-12 at 11:23 pm #38685
 SIPPAPAS WANGSRIParticipant
SIPPAPAS WANGSRIParticipantInteresting! I like how you address a preventive action. This kind of situation, especially sensitive information such as serological status of the patient must be kept securely and only authorised personnel can access. I guess as a system administrator, we are technically the most privileged users and that’s why we all have to abide by professional ethics!
-
-
AuthorPosts







