Forum Replies Created
-
AuthorPosts
-
-
2025-05-25 at 4:40 pm #48597
Ameen
Participant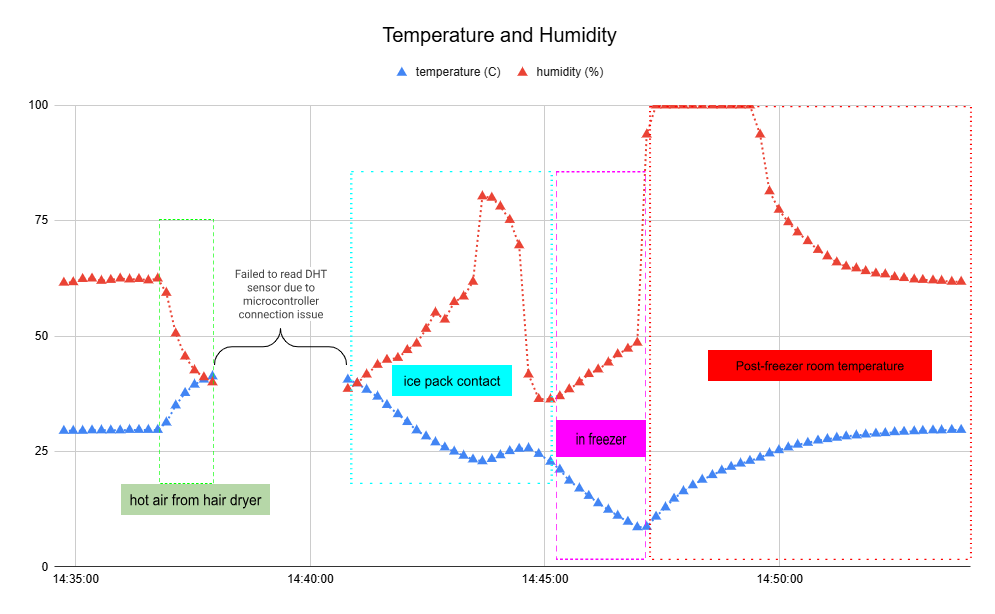
Challenges & Solutions
The ESP8266 initially failed to connect because it only supports 2.4GHz Wi-Fi—my first attempt used a 5GHz network. Switching to 2.4GHz resolved the issue. Later, applying hot air (~150°C) to the DHT22 sensor disrupted data logging. Even after stopping heat, readings didn’t resume until I reseated the sensor and USB connections, suggesting loose contacts from thermal expansion rather than sensor damage. This tells the need for secure wiring in high-temperature tests. The system now reliably logs data under normal conditions.Ideas for Improvement & Application
For this device, I’d use it to monitor bed temperature and humidity in nursing homes – especially for elderly patients who can’t communicate discomfort. We could set it up to text caregivers when readings hit levels that indicate irritation (like sweaty sheets or cold spots), so they can help before it becomes a real problem. -
2025-05-25 at 1:24 pm #48594
Ameen
ParticipantTitle: IoT garment for remote elderly care network
Authors: Francisco Luna-Perejón, Luis Muñoz-Saavedra, Jose M Castellano-Domínguez, Manuel Domínguez-Morales
URL: https://pmc.ncbi.nlm.nih.gov/articles/PMC9760329/1. Summary
This system uses a smart t-shirt packed with sensors (for temperature, heart rate, sweat, and motion trackers) to monitor the elderly remotely. It spots issues like falls, fevers, heart problems, or heatstroke and sends data to the cloud via the user’s phone. Caregivers get real-time alerts through an app.2. Key aspects
2.1 Objective
To monitor seniors’ health from afar. Detect problems early (weird heart rates, falls, etc.) and reduce in-person checkups workloads.2.2 Sensors Used
1) Skin temp sensor
2) Heart monitor (ECG)
3) Sweat sensor (GSR)
4) Motion detector (accelerometer)2.3 Challenges
The first prototype had stiff wires—they swapped them for comfy conductive thread. The sweat sensor had calibration issues, and the app confused some caregivers (no manual + older testers). Needs simpler visuals/docs. -
2021-01-24 at 8:01 pm #25566
Ameen
ParticipantThe topic #19 on page 343; The specific 95 % confidence interval presented by a study has a 95 % chance of containing the true effect size.
What I understand about confidence interval is it tells how much observed data (in percentage) that lie between a specific range of observed data from a group (either effect or control) of a study, while effect size is the size of the difference between two groups. So confidence interval has nothing to do with the chance of obtaining the true effect size as it represents only a group from the study.
For example, if the mean of observed data from a group in a study (either effect or control) is 80, with a minimum at 70 and 90 is a maximum, the observed data between the minimum and maximum would account to 100% of all observed data. So, 95% confidence interval would be that observed data that are within, for instance, 75 – 85 are account 95% of observed data on the group.
-
2021-01-03 at 11:18 pm #24883
Ameen
Participant1. Introduce yourself about your background, what kind of work you are doing that related to statistics.
I work for an insurance company’s claim department. My daily routine rarely uses statistic, except when I make a monthly/yearly claim payment report that I have to use some basic descriptive statistics.
2. Have you ever learned or applied statistics in your work related to data analysis or statistical analysis? Please share your experience.
I have never used statistic intensively with my work but now I am working on my personal project which to use the statistic for my proposal. The objective is to do a lean process. Since we have a lot of processes in claim settlement. Some are quite complex and lead to unsatisfied turnaround time. So, we will analyze the process to see if we can cut off any of sub-processor and develop new settlement method to make the workflow faster yet cost-effective.
-
2020-12-26 at 11:02 pm #24729
Ameen
ParticipantI think any study which has very specific participants or in small numbers must aware of the issue. For example, a study on the mental health of health professions in healthcare settings in levels/sizes which study areas and type of professions are stratified. Some study area may have only a healthcare provider and have only one staff for some specific health profession which is because of rare position or in a shortage situation such as a doctor, a medical/radiological technologist. Even the result shows only in the level of area and type of profession. The result may be identified directly to the participant because there is only a doctor in that whole area. Or any study which has small numbers of participants such as study using in-depth interview which normally recruits only a few subjects or studies in rare disease patients. When the report is made, the reader can immediately identify the subject based on the narrative written to explains the result and conclusion.
-
2020-12-19 at 12:07 pm #24588
Ameen
ParticipantIf the result is from a study in a rural area, I’d use Focus Group Discussion (FGD) combined with an in-depth interview to find out why they are not using bednets. First, I would do an IDI with key informants from the community such as village leader or village health volunteer on the general issue about the bednets in the community and also discussion about how to recruit community member who is not using bednets into the FGD. The two key informants also can help scope down the issues and give some guidance on how to conduct FGD appropriately regarding community character. The FGD may not be a typical conversational group interview, it can be activities with some entertainment or treat to make participants feel more informal and feel free to express their opinions and the root cause of the problem.
-
2020-12-13 at 10:25 pm #24452
Ameen
ParticipantReplacing technology might come with purposes such as cost reduction, version changes, contract changes or improved process requirement. According to TAM, apart from external variables, perceived usefulness is also influenced by perceived ease of use. If the user believes that the new one is easy to use, it can influence the belief that the new one is as useful as the old one. The new technology may not as useful as the old one when considering external variables but in the process of replacing, the organization may use intervention directly to perceived ease of use. It can directly influence the intention to use and is relative usefulness or is making user feeling that it is useful.
-
2020-12-13 at 4:26 pm #24449
Ameen
ParticipantIf the working-from-home system (set of hardware and software adopted to facilitate working from home) could be called a new technology, I think, Personal Life Affects and Primary System/Responsible Affects, might be some of the external factors that influence an individuals’ perceived ease of use.
Since the Covid-19 pandemic, I think many organizations have been struggling to adopt technology/system to facilitate their employee working from home. At my workplace, we have set up a system composed of a few hardware and software for that. It is sound good at first. Even it is on a voluntarily based, more than half of the staff requested to work from home. At beginning around 60% of the staff was working from home but now I believed more than 90% is working at the office. Apart from the fact that the pandemic in Thailand has been unfolding and it was not severe as expected, the reasons the working from home has been failed are mostly because of its effect on personal life and resources. Ranging from unable to manage work-life space at home, out-of-pocket for the system which not compensated by company i.e., internet subscription.
Lately, we have a survey on the issue as our organizational policy is heading to the working permanently for cost reduction. Some of the questions are if they would like to work from home or not and if not, what is the reason they do not want to. I do not know the result, but I speak with some staff and they disliked the WFH, in general, because the WFH systems which are a support system are not compatible with their primary working system/software/hardware. The performance of their primary system was affected as the system is compromised and unstable from some time. In the survey, I have given some comments that part from the system company should think about how to improve the working process and role and responsibilities altogether with adopting of system. The technology could not work well alone.
-
2020-12-05 at 1:54 pm #24241
Ameen
ParticipantA short explanation for the three terms can be explained by the drug developments/study. The three terms are used in a different kind of study during the development due to its different goals, tools, and messages the researcher wants to communicate.
‘Efficacy’ is a term used in the study under ‘ideal conditions’ such as in laboratory to answer the question of ‘What can the drugs do?’. For example, a study of how a phytochemical extract can inhibit the growth of tumour cells when managed in a test tube or ‘in vitro’, the result can be communicated by the efficacy of the extracts in inhibiting of the cells.
While, when the extracts showed expected sufficient ‘efficacy’, the next study can be to find the effectiveness of the extracts which produced in forms of drug and to be studied in ‘usual conditions’ or ‘real-life condition’. This is to answer the question of ‘What does the drug do?. The study can be a clinical trial in a selected healthcare setting or mass study in population. The drugs’ works would not only be between the extracts and the tumour cells anymore but involved by other factors such as conditions of the patient or dose management. The result can be expressed by the ‘Effectiveness’ of the drugs in the treatment of the patient with a tumour in different stages. The adverse outcomes are also the main interest in this kind of study.
‘Efficiency’ is mainly focused on resources/cost. The questions can be how does it takes/cost to make the drugs really work? For example, in a study, drug A show more effectiveness compared to drug B but it is more expensive. While the drug B require the patient to come to the hospital to get injected of the drugs and require for a one-night admission, the drug A which are in form of a tablet, the patient can take it at home following instructions and come to hospital only for following up. The evaluation considers the whole course which not only about the cost of the drugs but also the dose management, admission cost and other related costs/resources. When evaluated, drug B may have more ‘efficiency’ than drug A when considering the cost of the treatment comparing to the effectiveness of the drugs. The study can be to evaluate the ‘efficiency’ of the drugs for treatment considering many other aspects of health care or health system.
-
2020-12-04 at 12:10 am #24162
Ameen
ParticipantTitle :
Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailandhttps://wwwnc.cdc.gov/eid/article/26/11/20-3003_article
Main objectives of the study
To evaluate the effectiveness of personal protective measures against SARS-CoV-2 infections.Main exposure variable of interest
Both of the cases and the control groups were recruited from the contact tracing conducted by Surveillance and Rapid Response Teams of Thailand’s ministry of public health. All of the cohorts were asymptomatic at the time of recruitment.The variable of interest was maintaining of personal protective measures (mask-wearing, hand washing and social distancing) during the time having contact with the confirmed COVID-19 cases.
The main outcome variable of interest :
Case: Persons who tested positive for SARS-CoV-2
Control: Persons who were negative for SARS-CoV-2Limitations of the study
1. The cohort was recruited from 3 different settings which the result might not represent all the setting.
2. All of the cohorts were in contact with index cases. The analysis might not be an answer for another possible transmission in the community.
3. The controls cohort includes those who did not get tested due to the testing requirement, the low risk. They could have been infected. However, a small proportion of the group would not affect the result.
4. Since the contact record was self-reporting by the cohort, there might have missing of important contact or they might have contact with more than one confirmed cases.
5. Since the data collection was a retrospective; memory bias, observer bias, and information bias might occur. However, the interviewer was instructed to use structured interviews to reduce bias. -
2020-12-02 at 10:16 pm #24130
Ameen
ParticipantTitle :
Social Contacts and Mixing Patterns Relevant to the Spread of Infectious Diseaseshttps://pubmed.ncbi.nlm.nih.gov/18366252/
Main objectives of the study
To determine contacts patterns that relevant to infectious disease transmitted by respiratory or close contacts route.The sampling method used in the study.
This study was conducted in 8 European countries in a total of 7,290 participants. The participants were recruited by the quota sampling methodology and diary design. This way of sampling is intended to make proper distribution of samples in term of geographical spread, ages, and sex. However, for the age group, children and adolescents were deliberately oversampled, because of the important role of the group in spreading of infectious disease.Limitations of the study
The limitation of this study is that the data collected by self-reporting. The self-report based on each of the participant perceptions or called egocentric data which a subjective and might miss some data that no interest for the participants or deliberately missed out by the participants due to personal reasons. Another limitation is that there is variations of diaries report, recruitment procedure and follow up the process due to different commercial survey companies assigned to each country. -
2020-11-29 at 10:37 pm #24070
Ameen
ParticipantTitle
Facilitating the re-opening of Thailand with health IT if the vaccine is unavailable: Modelling of meta-population transmission dynamic of COVID-19 in the quarantine-free Thailand implementing of health IT involved strategies to cross border travel.General Objectives
To predict COVID-19 transmission dynamic in Thailand using mathematical modelling when health IT involved strategy is used as a public health measurement for reopening of Thailand to cross border travelling under the situation of unavailability of COVID-19 vaccine within two years and quarantine-free for inbound travelling is implemented.
Specific Objectives
1. To constitute and measure the effectiveness of an example of a framework for health IT using as part of the COVID-19 measures strategy for reopening of Thailand to cross border travelling under the situation of unavailability of COVID-19 vaccine within two years and quarantine-free for inbound travelling is implemented.
2. To predict COVID-19 transmission dynamic using mathematical modelling if the health IT involved strategy framework is used as a measurement for reopening of Thailand in cross border travelling under the situation of unavailability of COVID-19 vaccine within two years and quarantine-free for inbound travelling is implemented.
3. To predict COVID-19 transmission dynamic using mathematical modelling when the health IT involved strategy is used against different partner countries as measurement for reopening of Thailand to cross border travelling under the situation of unavailability of COVID-19 vaccine within two years and quarantine-free for inbound travelling is implemented. -
2020-11-14 at 2:02 pm #23865
Ameen
ParticipantI would like to raise “Being in higher education” as a confounder for this study. The young adult can be the group of people age 18-25 years old which mostly being in education ranging from advanced vocational education to undergraduate, postgraduate, and non-formal education and apprenticeships. This could be a criterion for confounder as “association”. While being in education requires them to have some certain frequent pattern of social contact or meeting between themself and group of people mostly with a classmate, institution staff, friends, colleague, and of using services. The contact and meeting mostly take place in public places like school, public transport, restaurant, class, shops. The places require them to use the contact tracing application. Moreover, being in education can lead to having collective and imitation behaviour. When one uses the app. the other will uses the app too. They ended up being recorded of their contact patterns. This could be “risk factors”. And being in education is not a by-product of being in any certain age group as not a derivative of growing into this group of age.
-
2020-11-08 at 11:08 pm #23766
Ameen
ParticipantProject: What do ‘Netizen’ aware and prefer toward the privacy of personal health data (PHD)?: Sharing of personal health data in health research and public health program via online-platforms.
1. Chosen choice of sharing of personal health data – Multiple categories variable – Summarized as proportion
2. Past participation in health research – Dichotomous variable – Summarized as proportion
3. Daily time spent online – Multiple categories variable – Summarized as proportion
4. Health status – Dichotomous variable – Summarized as proportion
5. Occupation – Multiple categories variable – Summarized as proportion -
2020-11-01 at 11:50 pm #23614
Ameen
ParticipantThe intervention I have added to my model is using health IT to support surveillance and monitoring of the disease. The intervention is characterised by its effectiveness tracing people how might be exposed to the viruses and also communicated with the target group through messaging features. The values used for the parameter is assumed to be 0.99.
-
2020-10-11 at 7:17 pm #23258
Ameen
ParticipantMY model will be a deterministic SIR model.
For the parameter, I am having difficulties finding and choosing the rights ones. The parameter I have chosen right now is as below.
Order|Variable name|Value or Range|Source of Information/Data
1|Basic Reproductive Number|3.75 1/day|Rotejanaprasert C. et al, 2020; (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7514043/pdf/pone.0239645.pdf) -
2020-09-17 at 10:01 pm #22590
Ameen
Participant1. Can family health informatics be done, in our context (Thailand)? What are hurdles to widespread implementations?
The article you picked up for presentation is focused on the child health the most. If this kind of study is to implement in Thailand, we should think about the elderly as we are heading to an ageing society. Elderly old is the most vulnerable in family and community, for me, more than children. Family is only one thing they can rely on when they are unable to live life on their own. The community in Thailand is not constructed and designed to support living alone as an older. Another social support like a nursing home or social security is still can’t keep up with the growing rate of older people. Only having good healthcare or good medical treatment system for older is not enough. Their health gradually deteriorates while they live longer with less support. There’s a study telling that if now you are under 40, you are likely to live longer to 100 years old! That’s so scary! The hurdles, if to apply to what I said, is about how policymaker and the society think about what it’s like being an ‘older’ in the country where majority is from low and middle income family. Is it only providing good healthcare and with 1,000-baht monthly allowance? How about social infrastructure for older empowering them to live and connect to their busy millennial decedent?
2. Can this be applied to community health? What are the similarities and differences?
It’s been recognized that Thai universal coverage and the successful in coping with covid19 in Thailand is a lot rely on community health in terms of people engagement. For me, community and family are the same, especially in a rural area. However, the sense of being in a community is strange. Community is like family, but you don’t want people in the community know much about you, while you may more comfortable to share your health status to people outside the community who you don’t know you. Community health informatics may be part of national health informatics in the sense of supporting community health practitioner to deal with health issue related to social factor and communicable disease in the community but not allowing people in the community to be able to access and use of the data on their own.
-
2020-09-14 at 11:55 pm #22493
Ameen
ParticipantThank you for the news sharing. I heard about the news that they are going to allow tourist to enter Thailand but limited to only Phuket. The tourist will need to stay quarantined for 14 days though! Meanwhile, in some European countries, they are thinking about reducing the number of days for the measurement. It’s quite interesting! We must reconsider the strategies to make sure the plan is worth to do. I am working on my project assignment and found some data will be needed. From the ministry of tourism, the average length of stay in year 2018 (data for 2019 was not completed) was only 9 days while among the top spender countries had stayed longer but with only 12 days in average.
For me, How many tourists will come to Thailand if they know that they will be required for quarantine for 14 days?
My ideas are we should not allow any countries else to come in with any numbers as much as they want. We should find country, regarding the infection rate in the country (to estimate how many people will already be infected when they enter TH) and how much will they spend during travelling in TH or in Phuket. They must be from the country where had low infection rate and stay longest (to have the least number of the country because it’s easier to deal with small number of home countries) and for sure are top spender.
-
2020-09-10 at 10:24 pm #22366
Ameen
ParticipantProject: Modelling of optimal quarantine strategies combine with measurements for Thailand reopening for tourist.
As of lately, from the news, some countries are considering reducing days of mandatory COVID-19 quarantine for the reopening country. The reducing may down to only at five days, as from the statistic, around half of infected persons showed symptoms at around day 5.
For Thailand, 10-15% of our GDP was from tourism and services industry; we should get ready for reopening our country to recover our economy. I think public health policy which lacking socio-economic perspectives will finally lead to another social problem and for sure, all policy implementing in national scale needs a lot of budgets. Any economic downturn will end up making the government losing income to support public health strategies. However, the reopening country can be an inevitably importing of infected persons. That is the reason we should be thinking about how to balance between the economic and the public health policy.
Questions I would like to raise for my projects regarding the mentioned ideas are;
1. How many days should be mandatory quarantine applied to the inbound tourist?
2. How many tourists should we allow to enter Thailand and from what country?
3. Apart from the compulsory quarantine what kind of other measurements/public health IT should we supplement to contain or mitigate the increased of infected person?
4. How is cost-effectiveness for each of measurement combination?Data requires the modelling of the reopening and combination of measurement.
1. Data from national case report for daily and accumulative incident recovered and deaths.
2. Data, the same as (1) for chosen countries.
3. Data for tourist spending for the past years.
4. Data for the effectiveness of each of measurement, strategies and health IT
5. Data for the latest update on incubation and infection period and transmission of the COVID-19.
6. And othersBasic Characteristic of COVID-19 which needed in the projects are;
1. Incubation period : 2-14 days (5% by 2 days, 50% by 5 days and 95% by 14 days)
2. Infectious period: 2 days before the start of sign and symptom to 10 days after onset of illness
– Asymptomatic can be infectious too.
– Most infectious at day 1 of symptoms onset.
3. Transmission :
– Viruses in mouth, nose and throat, droplet come out when talking, laughing, sneezing and coughing which can travel 6 feet away, then enter other’s noses, mouth and eyes.
– Viruses can stay on the surface then contaminate on the hands of others, washing and cleaning are important. -
2020-09-02 at 9:18 pm #22203
Ameen
ParticipantI would like to know how the movement restrictions or lockdown policy in countries worldwide help flatten COVID-19 epidemic curve and its effects on the economy. There are talk and argument about what is best when compared with economic loss. Comparing is, for example, Country closure vs internal closure, completely lockdown vs partial lockdown. In Thailand, I heard the news that they are going o open for a province for inbound tourist soon as the situation is getting better to help relieve the economic.
-
2020-08-13 at 7:36 pm #21628
Ameen
ParticipantI like looking at people doing the contact tracing when I go out. What I have seen in the public place where Thai Chana QR code is used, some visitor (quite a lot), even they have a mobile phone, they rather write down their phone number onto the signing book which is alternatives to the QR. And interestingly, I noticed that some person, they scanned the QR but not push it to the end, like they just pretended that they did just to be allowed to go into the place. For me, it’s interesting, they may concern about their privacy, or just don’t want to take more minutes to do it till finishes. As I said in the class, the app. was introduced to the public in urgent, and there was some weak point discussed in public by academics which might affect public perception or worse case, they scare of it already.
-
2020-08-05 at 11:16 pm #21309
Ameen
ParticipantI agreed we should start with fragmented first. As all of us look at the same way that the main barrier to implementing PHR is the low implementation of EMR in healthcare providers. Patients and the general public cannot clap one’s hands! While at the same time standalone PHR has an issue about data quality and meaningful use. I want to make it more clear about my idea in the seminar class. For me, starting with the general public is easier than the provider. The mass’s demands can trigger supplying of electronic data from the provider in addition to health data they already got from wearable devices daily. So the question is are there any system or if the HL7 can help transfer some medical data from the hospital’s system transferring to PHR (mobile app./web app)? It can start with only routine lab results or vital sign measured by the clinician. For example, I think lab results mostly has a fix report format/unit, easy to read, not like with hand-written in the doctor’s note. What if a PHR has a feature to extract data by the camera, from the paper-based report? With this way, without much effort from the healthcare provider and worker…they only have to hand over the patient the paper report for like few minutes for the patient to collect data.
-
2020-07-12 at 9:25 pm #20786
Ameen
ParticipantDiscussion 1
:: If I were the CDS developer I would add features that help physician give further advice on the due screening based on each of the patient, for example, where the patient can have the screening and help to make plans for the patient immediately on the visit. This may not be handled by the physician, it can be by other medical professions in the hospital after seen by a physician, to encourage the patients having the screening. After the recommendation and the plans have been made, there should have a reminder and following up from the hospital to make sure the patient get the screening following the plan. The CDS system will actively help improve the outcome of preventive services. The key point is HIE between hospitals and primary care, at least in regions where the patient lives.
Discussion 2
:: I think Thailand ้has made a good performance for health prevention. We have a wide primary care network which linked with hospitals. I heard that in the budget per head from UHC, the budget for preventive care has been added. In the year 2020, the budget even managed for PrEP program for HIV prevention. I think if the CDS is developed not only to help remind physician but on the ideas of to enforce the preventive care throughout the system via HIE, the good outcome is to be expected. Like I said earlier, a recommendation made by a physician may be transferred to another healthcare worker to make sure the procedure is done.
-
2020-07-12 at 6:23 pm #20784
Ameen
ParticipantTopics 1 Good electronic system come with the price, how do we develop it in a low resource country like Myanmar?
In Thailand, we also have to deal with low resources setting. I think sharing of resources and networking between the low-resources and high resources is a way to do. Apart from the governmental level, organizations in Myanmar, both public and private may make network with the same kind of organization in its regional neighboring country. The networking is not only to share or find out resources but also to make information exchange across the region which very important and is an ultimate goal for using the electronic system.
Topics 2 How do we manage the capacity of staffs with high turn-over rate?
At work, I also have a problem with a high turn over rate. In exit interview, the feedback we got from the staffs was mostly about career development and support at work. As in a supervision level, what I recommend is a coaching one-on-one. For me, coaching is not only about things to do at work but also how they can live their life with the work. It’s more than work. So If we talk about the capacity of staff, we should not only talk about their skills for the certain job but also their ability to balance their work and life and the career development both in a short and long term. Especially, in low resources setting, work may take their personal life like working late due to insufficient support or workload or shortage of resources may cause burnt out. You also have to look at their generation, the gen. Y-Z want more independent life with quick success in work. Your coaching may focus on very of dimensions.
-
2020-07-12 at 4:51 pm #20783
Ameen
Participant1. What is your opinion about Concentrations of SO2 in the resident more than the workplace.
ANS. We don’t know much, from the article, about Jinan in terms of air pollution background. China’s industrialization has been so fast. The article used data in the year 2009 which a decade ago. Not sure if in Jinan, back then, the main industry was off any main sources of SO2 and how was the household behaviour in Jinan. As we know the most sources of SO2 are from the burning of fossil fuels like using coal for heating and cooking in the household or coal and oil in powerplant. Back then China was in needs of power for industry development and for sure coal and oil were the main sources. And as K’ Thanachol said, from the article, SO2 both in domestic and workplaces have significantly correlated to the hospitalization. However, we still don’t know much about their household and workplace in details. From the subject’s age, very old, the missing in this article is what kind of work the subject do for a living and type of housing they lived in. These might affect the degree of exposing to SO2 both in terms of geographical, work type and individual factors.2. What do you think about this paper to improve paper adapts to Thailand.
ANS. We should have this kind of research more to present to decision-maker officials. Creating the new industrial estate has been proposed by the government and as we all know, this kind of project has never been planned and managed well to prevent air pollutions. This kind of study could help to monitor the existing issue and draw attention to the public and government to be always aware of the pollution. -
2020-07-11 at 1:39 pm #20763
Ameen
ParticipantAj. Saranath, Thank you for your comments and suggestions. I have changed the header’s font, from white to black with white frame and shadow. It looks better indeed.
-
2020-07-06 at 5:56 pm #20671
Ameen
ParticipantSorry, everyone, please ignore the link of my dashboard above and instead visit the one here :
-
2020-07-06 at 5:44 pm #20670
Ameen
ParticipantPlease visit my dashboard at :
My dashboard, part from showing numbers of confirmed cases, deaths and recovered cases the same as other’s including the overall situation, I tried to visualise workload and proportion of cases comparing between continents and countries. In addition, I wanted to use some of the economic and demographic factors which are GDP, population, and GDP per capita, to present the severity of PH workload in countries. This is intended to present where are the most in need of public health and international aids to fight the public health emergency. In some countries, reported cases are not on top rank but if we compare with its population and its economic background referring to the GDP per capita. For example, if we look at countries where GDP per capita lower than 40,000 USD, Brazil, India, Russia, Chile and the UK are countries where international organizations should pay attention to. Especially, when looking at forecasting of new daily confirmed cases which tend to increase steadily.
-
2020-07-05 at 4:19 pm #20668
Ameen
ParticipantPlease visit my week 4 dashboard here: My Dashboard
On the Global summary, the map and card are used to present the overall quick summary of confirmed, deaths and recovered of COVID-19.
On the deaths and recovered, the scatters plot and funnel chart is used to present situation of the recovered by country compared to its cumulative cases whiles the funnel sum up deaths numbers worldwide by month showing decreasing of deaths.
The last, the treemap is used to present the proportion of confirmed case by continents classified by country.
-
2020-07-02 at 10:44 pm #20514
Ameen
ParticipantPlease ignore the above-broken link and refer to this one instead.
-
2020-06-26 at 10:58 pm #20461
Ameen
ParticipantMy dashboard : shorturl.at/beqHL
My dashboard composed of 6 sections.
Section 1: Use Area Chart to visualize global total confirmed case, deaths, and recovered of COVID-19 over time. This chart help viewer comprehends the overall situation of COVID-19.
Section 2: Use Line Chart to visualizes daily cases per million of the population by continents over time. This will help the viewer comprehend not only cases by number but by prevalence. In addition, using stacked and clustered column chart help the viewer be able to compare daily confirmed cases and accumulated cases overtime. Overall, the donut chart shows the percentage of confirmed case sharing by continents.
Section 3: Use stacked bar chart together with scatter plot to specifically present situation by countries based on confirmed cases and deaths per million of populations.
Section 4: Use Line chart with forecast to predict the situation in the next 10 days for confirmed cases, deaths and recovered of COVID-19.
Section 5: Use sparkline chart to show the pattern of daily confirmed cases based on population and GDP selected by the viewer.
Section 6: Use 100% stacked bar chart to show the percentage of confirmed cases, deaths and recovered of covid19 by countries. -
2020-06-20 at 8:58 pm #20266
Ameen
ParticipantPlease find my dashboard here : https://app.powerbi.com/view?r=eyJrIjoiMjlkYzYxMTUtNjc1NC00Y2M1LWEyZjYtZjUxZTBmYTc2M2Q2IiwidCI6ImE1NjYxYjU3LTQ3ZDItNDNlNC04MGFhLWYxNzcwMTZhNTJmYiIsImMiOjEwfQ%3D%3D
The first table : Daily statistic by country. By filtering, user can check confirmed, death and recovery cases on a daily basis.
The second table : Accumulative cases by country to see cases in total till date for each country. In this table I am not sure how to make accumulative sum of cases so I use the maximum.
The third table : World GDP by country and continent. -
2020-06-07 at 9:47 pm #19955
Ameen
ParticipantHi Khun Chanapong….In addition to what Ah.Saranath mentioned, I found your dashboard is “Fun”. They offer options for us to change the chart type when maximizing the chart too. I think this is good for the viewer to make their own chart to find insights.
-
2020-06-07 at 9:37 pm #19954
Ameen
ParticipantHi Thansoeoosoe.Oo … I like the interactive describing data when pointing out at every single point in the graph, also the graduated point map to distinguish between total confirmed cases and per million population for each country. The thing that not quite appropriate, for me, is that the class values are not proportional. Maybe because of the wide ranges of total confirmed cases worldwide. However, they should have given a legend for the graduated point map.
-
2020-06-07 at 8:40 pm #19953
Ameen
ParticipantKhun Tullaya, Your dashboard has given overview insights in terms or global situation yet minimalized. I like the stacked histogram showing case comparison by WHO Regions. It gives a one-shot insight into how much burden America and Europe has for the situation compare to other regions.
-
2020-06-06 at 11:16 pm #19940
Ameen
ParticipantI am quite sure all dashboards shared by our classmate are impressive and has many options to be an example to be used in the future. However, I would like to show the one that I DON’T LIKE, just to give an example of what I think is not an example of a useful dashboard. The one I am talking about is from Thailand’s department of disease control. You can check out at the site : https://ddc.moph.go.th/viralpneumonia/index.php
This supposed to be the most referred dashboard in our country as the data is verified by the national authority. There is some point I would like to mention that making this dashboard being as not as good as it supposed to be.
1. There is no graphic used to distinguish each variable and data. Only letter and numbers are used to present the data which is not attractive and not trigger the iconic memory of the viewer. This is the main issue making this dashboard a weakness. It increases the time to insight for the viewer. They should have added histogram or lines to show trends. Also, cases by province are necessary for viewers to make the decision for travelling or activities based on the cluster.
2. The colour theme, which is pink is unusual for use in academic or in data that need to be trustworthy. Most dashboards use blue and red as the main colour theme, which is more “powerful” and more trustworthy. They should use primary colour (Blue, Red, Yellow) or secondary colour (Green, Orange, Purple). In term of the electromagnetic spectrum, pink is not colour at all as there is no pink light. So not a good colour to catch up.
3. The contrast between the font and the theme is difficult to differentiate especially, white font with a light pink background.
4. There is a section which consumes half of the dashboard which I think is not necessary or at least no need to take that much area. It’s the “Travelers Screening at Ports of Entry”. This may be an attempt to restore the credibility of the authority as at the beginning they were criticized for being unable to control the border, which made a lot of imported cases.
5. In the Thai language version, they use a reduced-head Thai font which is not a standard font and hard to read for some age group. -
2020-05-26 at 9:05 pm #19607
Ameen
ParticipantHi Khun Kunnthida…The study concludes only people are diagnosed with TB, both newly and previously. The result is to find out a potential risk of TB transmission in a school.
-
2020-05-23 at 10:47 pm #19565
Ameen
ParticipantHi Khun Chanapong…I am not an expert in the US health care system too but from I heard, population +65 in the study should be covered by “medicare”, the insurance scheme for old age. However, not all older covered by the scheme, some may be covered by self-funded private insurance. I just google about the coverage and found that medicare cover EMS both emergency and non-emergency under some circumstances. You may find below. However, uninsured in the US is a lot and has been criticizing. There is a fraction of system and mostly private even the medicare/medicaid.
To re-design this study, they may add more layer by mapping with insurance data for every EMS call to find a correlation between increasing of call in each sub-socio-economic group.
Does Medicare cover ambulance services?
https://www.medicareresources.org/faqs/does-medicare-cover-ambulance-services/ -
2020-05-23 at 12:11 am #19529
Ameen
ParticipantHi Khun Thanachol… Thank you for your presentation. You gave all details from the study to us in depths. I have something I don’t understand much which is because myself and it’s about statistical analysis. A conclusion is most of the crashes happened on the high way where mostly direct route which I think apparently all high way is a direct route by nature not an area like communities. Why do we need clustering analysis? What’s the importance of the Moran I index and why this study needs it?
Thank you so much for your good work.
-
2020-05-22 at 11:27 pm #19527
Ameen
ParticipantHi Khun Chanapong…Thank you for the presentation. This study reminds me of our UHC. When the UHC had been implemented, the number of patients visiting hospitals kept increasing significantly and some say that it’s because of the free of charge so coming to the hospital is not to worry much about anymore. But that fact is, the UHC fulfil the missing gap between the demands and the supply of services by getting the financial barrier off. Not because it’s free of charge so people keep coming to the hospital.
In the US, as I know calling EMS is not for free. It can cost a huge amount of charge. Apart from the fact that, as you mentioned, the participant might be given the knowledge to call EMS so they cal more, do you have any suggestions on socio-economic demographic and financial factors that made the calls increased every year? Does the study design have any opportunity to map such factors more on the existing layers?
-
2020-05-22 at 10:06 pm #19523
Ameen
ParticipantHi Khun Chalermphon….The objectives of this project are what we want to escalate the air pollution situation to national level or national agenda. I have to say that statistic is not my cup of tea but I always want to know about it. This study picked up data for all the parameters only during Jan – April, which I assume because of the reason of the agricultural burning causing air pollution. I wonder if the study picked up data throughout the years, when the air pollution, the PM10 steadily decreased to almost not an impact to air quality when the agricultural and rainy season comes. would the correlation of the PM10 and influenza and pneumonia be effected?
Thank you for your presentation krub!
-
2020-05-21 at 11:08 pm #19485
Ameen
ParticipantVideo Presentation
-
2020-12-23 at 10:03 pm #24681
Ameen
ParticipantAgreed, in interviewing, sometime participant doesn’t aware or may deliberately omit about an important topic which could lead the researcher to the root cause. Observation can help resolve the bias. I think if researchers want to do the method they should have a plan about the period of time for the observation and how they could be part of the activities without interfering. The participant may not act like in everyday life or ‘get everything ready to be seen’ if they know beforehand about the study. In interviews, the participant may not naive and would speak out only what likely to reflect a good image of them.
I used to have fieldwork on the dietary pattern. Instead of interviewing on the pattern, we join the cooking time and observe how and what they use in cooking such as the portion of seasoning or eating portions.
-
2020-12-17 at 10:29 pm #24577
Ameen
ParticipantAn external factor that I can think about apart from what explained in the TAM2 is TIMELINESS. The WFH system has been introduced for a long time but immediately getting popular because of the pandemic. It has been cleared because of perceived usefulness.
People decided to take the WFH because they thought it is useful. When they have experience using it, they faced some difficulties and stop using it because of the perceived ease of use. -
2020-09-05 at 9:24 pm #22257
Ameen
ParticipantThank you for your feedback Aj,Pan.
-
2020-09-03 at 9:45 pm #22218
Ameen
ParticipantThank you for letting us know super cool dashboard!. So this is a usage of mathematic modelling? I tried the simulation and it’s very useful and that some countries already made the decision based on this. Where can we find the model used for the simulation? I noticed that it’s also open data.
-
2020-06-07 at 8:29 pm #19952
Ameen
ParticipantThank you, Aj.Saranath for your suggestion. I checked out the dashboard and found it’s quite good but have it could have been better if;
1. They could replace the table with a list of confirmed cases by province with a horizontal bar graph. Also, the list should be on one page, by stretching down to the bottom.
2. In the map, they could use the graduated point map to show cumulative and active cases in real-time.
3. In the population statistic, using the stacked histogram for age and sex can show overall insight which is better than knowing the average, minimum and maximum age.I found there is actually another dashboard which looks like a JHU’s dashboard but in version from the department of disease control. The site is https://ddcportal.ddc.moph.go.th/portal/apps/opsdashboard/index.html#/20f3466e075e45e5946aa87c96e8ad65 It will be great if they can combine the two.
-
2020-05-23 at 10:25 pm #19563
Ameen
ParticipantHi Pyae Phyo Aung…Thank you for your questions. I have to accepts that this study is huge and there are numbers of the previous study by Wood et al to read more. However, I am making myself to get to understand the concepts in a limited time and here is my answer.
Refer to Table 1, only 3 out of 36 subjects from new and previous TB who go to school while the rest are in the working group or unemployed.
Apart from the RAVS, the factors that make a place a potential risk is a number of people sharing rooms at the time with. The new and previous TB share room with other less than adolescents, from the study in Table 1, there are significant difference of cohabitees for the new TB, previous TB and adolescent groups (1.5, 2.8, 3.7 respectively; p = 0.004) and mean numbers of those sharing a room to sleep (0.4, 1.2, 1.4 respectively; p = 0.024). This may be because of the awareness in the household, the infectious person is informally separated at household. While in adolescent, RAV at household much less than at school (13.69, 71.26). Simply put, at households there is less chance for adolescents to inhale TB infectious air compare with at school. In the study, they said, Schools have long been recognized as sites of TB transmission (Bates et al., 1965) due to building ventilation, classroom occupancy and exposure times which are encapsulated in RAV measurements. Apart from air cleaning, designing of the classroom should pay attention more on such element to prevent transmission of infectious disease not only TB but others too.If my understanding is working please don’t hesitate to correct me.
-
2020-05-23 at 3:56 pm #19554
Ameen
ParticipantHi Khun Patcharapol…Thank you for your comments. The device used in this study reminds me of contact tracing application too. Imagine, our mobile phone which already has ability to do the GPS tracking can have more biomedical function like the CO2 levels monitoring installed in. I used to read an article about ideas of developing our mobile phone to have some medical function for telemedicine/public health. What if the mobile phone can “SMELL” viruses from its derivatives/ by-product/excretion from an infected person while at the same time mapped with the location where it smells!
-
2020-05-23 at 3:43 pm #19552
Ameen
ParticipantHi Khun Chanapong … Thank you for your comments. According to my understanding…This study is interpreting hot spot analysis to find exposure potential for the susceptible and transmission potential regarding adolescents. Results in Fg.2 B shows that adolescents spent more than halves of time throughout the study at school/work. The transmission potential risk is where the subjects spent high RAVs or inhale a lot of sharing exhaled air with other people for a long period of time. While the informal household and combined housing, which not where the susceptible group spend much time. The hot spot analysis uses Getis-Ords Gi*statistic. I may not be able to explain the analysis in details but you may find in additional here: https://pro.arcgis.com/en/pro-app/tool-reference/spatial-statistics/h-how-hot-spot-analysis-getis-ord-gi-spatial-stati.htm.
-
-
AuthorPosts
